Critical Care & Resuscitation Research
The Division of Pulmonary, Critical Care, and Sleep Medicine conducts research in clinical critical care, critical care physiology, cardiac arrest, post-resuscitation care, and observational and interventional studies in patient with critical illness related to 2019 coronavirus disease (COVID-19). We also create simulations designed to improve critical care outcomes.
Critical Care Clinical Research
David A. Kaufman, MD, is principal investigator of several of NYU Langone’s ongoing critical care research projects. He has a number of specific interests:
- understanding 2019 coronavirus disease (COVID-19)–related critical illness
- understanding lung mechanics in patients with respiratory failure to improve patient comfort and outcomes in those requiring mechanical ventilation
- identifying patients at high risk for developing acute respiratory distress syndrome, with the goal of implementing strategies to decrease its incidence and severity
- improving shock resuscitation through a better understanding of the use of intravenous fluids
Recent Publications
Jay Chandra, Miguel A Armengol de la Hoz, Gwendolyn Lee, Alexandria Lee, Patrick Thoral, Paul Elbers, Hyung-Chul Lee, John S Munger, Leo Anthony Celi, David A Kaufman. A novel Vascular Leak Index identifies sepsis patients with a higher risk for in-hospital death and fluid accumulation. Crit Care. 2022 Apr 11;26(1):103. DOI.
Anthony Steven Lubinsky, Shari B Brosnahan, Andrew Lehr, Ola Elnadoury, Jacklyn Hagedorn, Bhaskara Garimella, Michael T Bender, Nancy Amoroso, Antonio Artigas, Lieuwe D J Bos, David Kaufman. Inhaled pulmonary vasodilators are not associated with improved gas exchange in mechanically ventilated patients with COVID-19: A retrospective cohort study. J Crit Care. 2022 Jun;69:153990. DOI.
Ivor S Douglas , Philip M Alapat, Keith A Corl, Matthew C Exline, Lui G Forni, Andre L Holder, David A Kaufman, Akram Khan, Mitchell M Levy, Gregory S Martin, Jennifer A Sahatjian, Eric Seeley, Wesley H Self, Jeremy A Weingarten, Mark Williams, Douglas M Hansell. Fluid Response Evaluation in Sepsis Hypotension and Shock: A Randomized Clinical Trial. Chest. 2020 Oct;158(4):1431-1445. DOI.
Critical Care Physiology Clinical Studies, Humanization Studies, and Ethics
Jan Bakker, MD, PhD, principal investigator, has numerous research interests in critical care medicine and cardiopulmonary physiology, the hemodynamics of sepsis, hemodynamic effects of mechanical support of the circulation, ethics and humanization studies
Dr. Bakker has a number of active research projects:
- COVID-19 and diastolic shock index, blood volume, ferritin levels, lactate levels, and cause of death among other topics
- peripheral circulation as an endpoint of resuscitation in septic shock patients
- effect of mechanical support of the circulation on the microcirculation in patients with circulatory failure
- effect of early standardized fluid resuscitation in patients with severe sepsis on peripheral perfusion and lactate levels
- early use of a vasopressor with limited fluid resuscitation in septic shock patients
- cardiac dysfunction in septic shock and the effect of raising blood pressure on cardiac function parameters
- reluctance to admit patients with hematological malignancies to the intensive care unit (ICU)
- post-intensive care syndrome (PICS) in ICU patients and family members in Latin America
- effect of the social and economic context of the patient and family on PICS in Latin America
- organizational and economic consequences of ICU waste
- end-of-life care in critically ill
Recent Publications
Zampieri, F. G., L. P. Damiani, J. Bakker, G. A. Ospina-Tascon, R. Castro, A. B. Cavalcanti, G. Hernandez, Andromeda-Shock Investigators, and Network the Latin America Intensive Care. 2020. Effects of a Resuscitation Strategy Targeting Peripheral Perfusion Status vs Serum Lactate Levels Among Patients with Septic Shock: A Bayesian Reanalysis of the ANDROMEDA-SHOCK Trial. American Journal of Respiratory and Critical Care Medicine, 201: 423-29.
Wernly, B., N. Heramvand, M. Masyuk, R. Rezar, R. R. Bruno, M. Kelm, D. Niederseer, M. Lichtenauer, U. C. Hoppe, J. Bakker, and C. Jung. 2020. Acidosis predicts mortality independently from hyperlactatemia in patients with sepsis, European Journal of Internal Medicine.
Squara, P., T. W. L. Scheeren, H. D. Aya, J. Bakker, M. Cecconi, S. Einav, Mlng Malbrain, X. Monnet, D. A. Reuter, I. C. C. van der Horst, and B. Saugel. 2020. Metrology part 1: definition of quality criteria. Journal of Clinical Monitoring and Computing.
Bakker J, Postelnicu R, and Mukherjee V. Lactate: Where are we now? Crit Care Clin. 2020. DOI.
Trogrlic Z … Ista E. Improved guideline adherence and reduced brain dysfunction after a multicenter multifaceted implementation of ICU delirium guidelines in 3,930 patients. Crit Care Med. 2019. DOI.
van den Akker JPC … den Uil CA. Risk indicators for acute kidney injury in cardiogenic shock. J Crit Care. 2019. DOI.
Verkerk BS … Bakker J. Opioid and benzodiazepine requirements in obese adult patients receiving extracorporeal membrane oxygenation. Ann Pharmacother. 2019. DOI.
Cardiopulmonary Resuscitation Research Program
Led by Sam Parnia, MD, PhD, at the Parnia Lab, the mission of the Cardiopulmonary Resuscitation Research Program is to improve the survival and functional outcome of people experiencing cardiac arrest and post-cardiac arrest syndrome. This is a complex cascade of biological events that follows the restoration of the heartbeat and circulation and contributes to organ injury, including persistent disorders of consciousness. Our approach involves identifying and encouraging ever-improving methods to prevent premature death and decreasing associated disabilities from cardiac arrest.
The work of this program includes an international, multicenter cardiac arrest study that is being conducted by an interdisciplinary team. Our areas of research interest include the following:
- trials to evaluate treatments for COVID-19
- methods to measure and improve brain resuscitation during CPR
- models to predict cardiac arrest survival and neurological outcome
- neuroimaging of brain injury after CPR
- neuroprotective strategies after CPR
- biomarkers of organ injury after CPR
- quality of life in cardiac arrest survivors
- mechanisms underlying various states of consciousness during and after resuscitation
- qualitative studies of the experience of death
This is the first research program in New York City dedicated to saving the lives and brains of people with cardiac arrest and shedding light on what happens when we die.
Recent Publications
Guidelines and standards for the study of death and recalled experiences of death—a multidisciplinary consensus statement and proposed future directions. Ann N Y Acad Sci. 2022;1511:5-21.
2021 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Neonatal Life Support; Education, Implementation, and Teams; First Aid Task Forces; and the COVID-19 Working Group. Circulation. 2022;145:e645-e721
Pharmacologic neuroprotection in ischemic brain injury after cardiac arrest. Ann N Y Acad Sci. 2022;1507:49-59.
Cerebral oximetry: a developing tool for monitoring cerebral oxygenation during cardiopulmonary resuscitation. Ann N Y Acad Sci. 2022;1509:12-22.
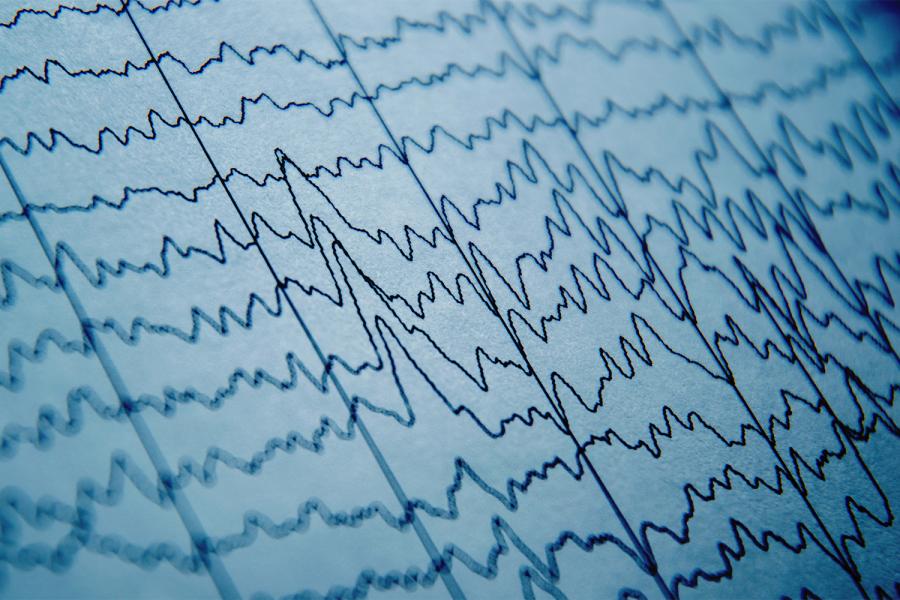
Monitoring the Relationship Between Changes in cerebral Oxygenation and Electroencephalographypatterns During Cardiopulmonary Resuscitation. Critical Care Medicine. 2018; 46:757-763.
Monitoring the Brain After Cardiac Arrest: A New Era. Curr Neurol Neurosci Rep. 2017;17:62.
Cerebral Oximetry During Cardiac Arrest: A Multicenter Study of Neurologic Outcomes and Survival. Critical Care Med. 2016;44:1663-74
Critical Care Simulation
Simulation, an important tool in the training and education of practicing physicians, allows trainee physicians to learn new procedures and clinical teams to practice the management of critically ill patients without risk of patient harm.
The simulation research team, led by Brian S. Kaufman, MD, takes on a third-year fellow each year to develop a research project involving ways in which simulation can improve critical care patient outcomes. The team includes Kevin J. Felner, MD, and Anthony Andriotis, MD.
Recent Publications
Mitchell O … Madeira C: Development and evaluation of a cognitive add booklet for use in rapid response scenarios. Simul Healthc. 2019. DOI.
Zachary BM … Felner KJ. The utility of high-fidelity simulation for training critical care fellows in the management of extracorporeal membrane oxygenation emergencies: A randomized controlled trial. Crit Care Med. 2017. DOI.
Greenstein YY … Kaufman B. Goal-directed transthoracic echocardiography during advanced cardiac life support: A pilot study using simulation to assess ability. Simul Healthc. 2015. DOI.