Rusk Rehabilitation Education & Research

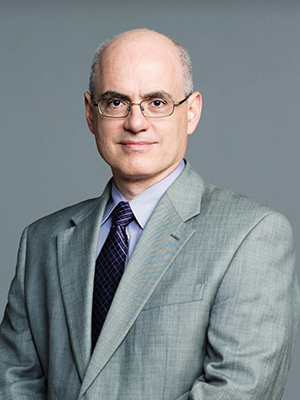
Steven R. Flanagan, MD
Chair, Rusk Rehabilitation
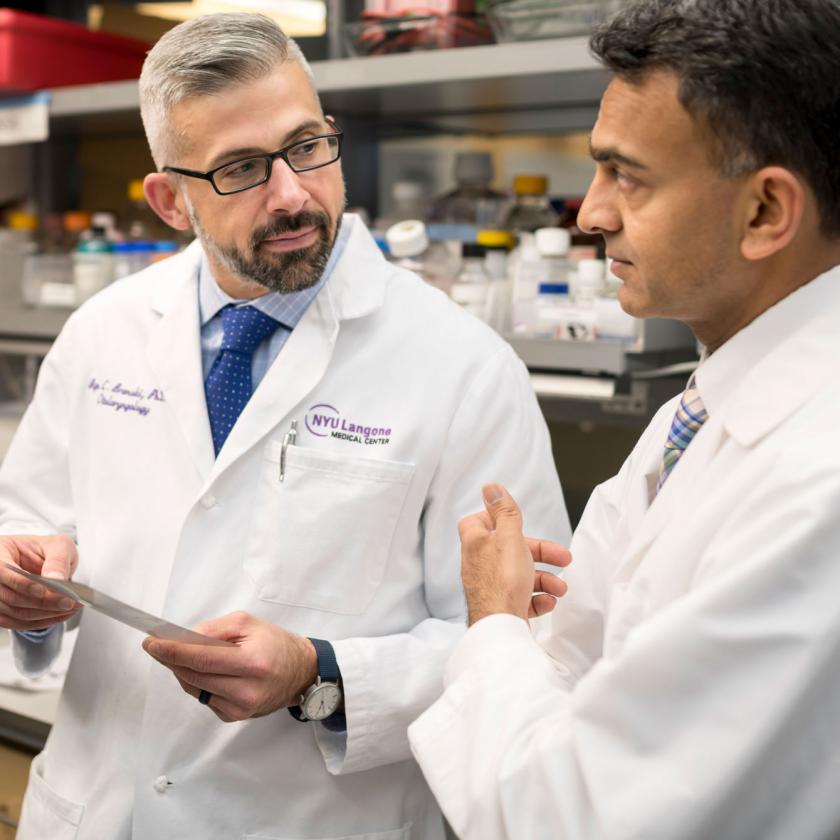
At NYU Langone Health’s Rusk Rehabilitation, we offer physicians, researchers, fellows, residents, therapists, neuropsychologists, and medical students a broad scope of educational, research, and clinical programs at multiple locations.
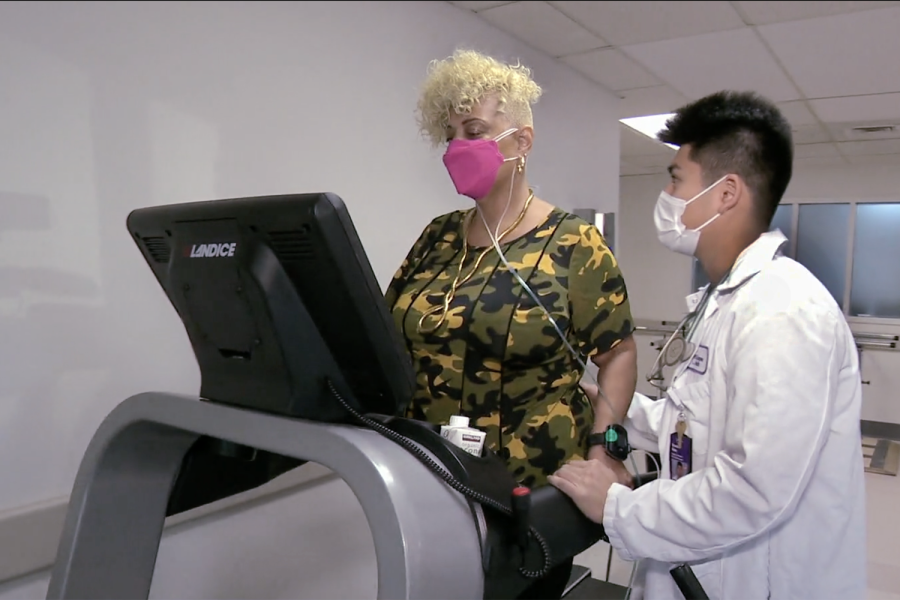
We provide a full spectrum of inpatient and outpatient rehabilitation care to people of all ages for a wide range of conditions and injuries, including cardiac, neuromuscular, oncologic, musculoskeletal, pulmonary, and stroke.
In addition to our tremendously talented physicians and nurses, we have a terrific group of therapists, social workers, and support staff—all of whom are ready to prepare the next generation of rehabilitation specialists. We encourage you to explore the various opportunities to train at one of the most renowned rehabilitation locations in the country.
We are proud to belong to a worldwide rehabilitation community that is dedicated to making sure patients not only survive but also thrive and achieve their greatest potential. As we look to the future, we plan to continue to expand access to rehabilitation medicine, engage in valuable research, and exercise our passion for restoring our patients’ abilities.
Ranking, Accreditations, and Awards
U.S. News & World Report has ranked Rusk Rehabilitation as one of the top 10 rehabilitation programs in the nation since 1989. It is home to innovations and advances that have set the standard in rehabilitation care for every stage of life and phase of recovery.
Rusk Rehabilitation at NYU Langone Hospital—Brooklyn boasts an inpatient 30-bed adult rehabilitation unit, which is a stroke rehabilitation Joint Commission–accredited site.
Our acute rehabilitation program at Tisch Hospital and our brain injury rehabilitation, stroke rehabilitation, and pediatric rehabilitation programs at NYU Langone Orthopedic Hospital have been accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF).
Rusk Rehabilitation was among the first hospitals in the nation to earn a three-year CARF accreditation for a stroke specialty program. We are home to 1 of only 16 traumatic brain injury model systems in the country and only 1 of 2 in New York state funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR), a component of the U.S. Department of Health and Human Services and the main federal agency that supports applied research, training, and development to improve the lives of individuals with disabilities.
Our program has also earned Magnet® recognition for excellence in nursing from the American Nurses Credentialing Center (ANCC) and The Gold Seal of Approval® from The Joint Commission for our commitment to providing our patients with the highest-quality care.
Our Educational Opportunities

Our Research
Events
Continuing Education

Our top podcast offers a close look at what is transpiring in rehabilitation research and clinical services.
Learn More
Doctor Radio

Related News

Dog Helps Boy in Physical Therapy After His Surgery

Rusk Marks 75 Years of Rehabilitation Innovation

Rusk Rehabilitation Is Still at Its Best After 75 Years
Brooklyn Resident Fights Lingering Symptoms of Long COVID

Reducing Risk of Bone Fractures in Older Cancer Survivors

Pilot Program Offers Virtual Supportive Oncology Visits

Rusk Rehabilitation Patient Returns to Accident Site

Computer Tool Can Track Stroke Rehabilitation

Brain Surgery & Rehabilitation Save a 13-Year-Old’s Life

Research Examines Swallowing Problems After Spine Surgery

Face & Double Hand Transplant at NYU Langone Is Successful


