Colton Center for Autoimmunity Research
At NYU Langone’s Judith and Stewart Colton Center for Autoimmunity, our researchers conduct pilot projects and collect data for biomedical research to better understand the immunological basis of autoimmune disorders.
We pioneer basic science and translational research that drives advances in the diagnosis, treatment, and prevention of autoimmune diseases, such as ankylosing spondylitis, antiphospholipid syndrome, arthritis, lupus, Sjogren’s syndrome, and type 1 diabetes.
Learn more about our work by reading the latest papers published by our investigators.
2024 Grant Awards
Researchers at NYU Langone’s Judith and Stewart Colton Center for Autoimmunity are advancing the understanding and treatment of autoimmune diseases. Their studies range from exploring immune response mechanisms in organ transplants to developing innovative diagnostic tools for early autoimmune disease detection.
Blocking Copper Transport in Multiple Sclerosis Treatment
Principal Investigator: Stefan Feske, MD
The goal of this project is to understand how a protein called SLC31A1, which helps transport copper in the body, affects the behavior of Th17 immune cells that are known to cause inflammation in the central nervous system during autoimmune diseases like multiple sclerosis (MS). Using mice with inducible deletion of SLC31A1 in the experimental autoimmune encephalomyelitis (EAE) model of MS, this project assesses if blocking copper transport is a new approach to MS therapy.
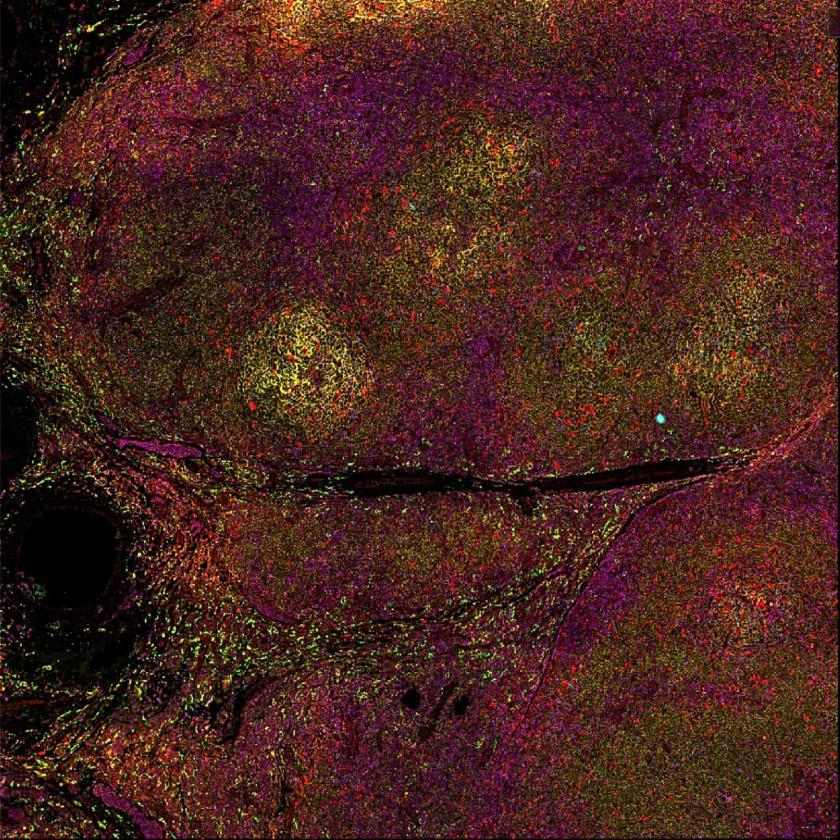
Targeting Allograft Inflammation with CAR Tregs in Transplantation
Principal Investigators: Marlena Habal, MD; and Mark Yarmarkovich, PhD
There is an urgent need to improve how we manage immune response to organ transplants without relying heavily on immune-suppressing drugs. The approach in this proposal involves developing specialized immune cells (CAR Tregs) that can specifically target areas of inflammation around transplanted organs and inflammatory diseases. We seek to understand how these cells function in different conditions, allowing for more effective immune response control in cases of transplant rejection and autoimmune diseases.
Development of Rationally Designed PD-1 Agonist Biologics for the Treatment of Autoimmune Diseases
Principal Investigators: Xiangpeng Kong, PhD; Jun Wang, PhD; and Elliot Philips, MD, PhD
New PD-1 antibodies show potential in treating autoimmune diseases by calming overactive T cells, though their effects remain modest. These antibodies bind to the lower part of the PD-1 protein on T cells, but their efficacy is limited by the need for Fc receptor engagement. Recent research from our team demonstrates that PD-1 proteins naturally pair (a process called dimerization) through transmembrane domain interactions, with dimerization correlating with T cell inhibition and immune tolerance. This study aims to develop new antibodies that target this specific area near their membrane-proximal stalk region (MPSR) to more effectively suppress T cell activation in rheumatoid arthritis, systemic lupus erythematosus, and other potential autoimmune processes.
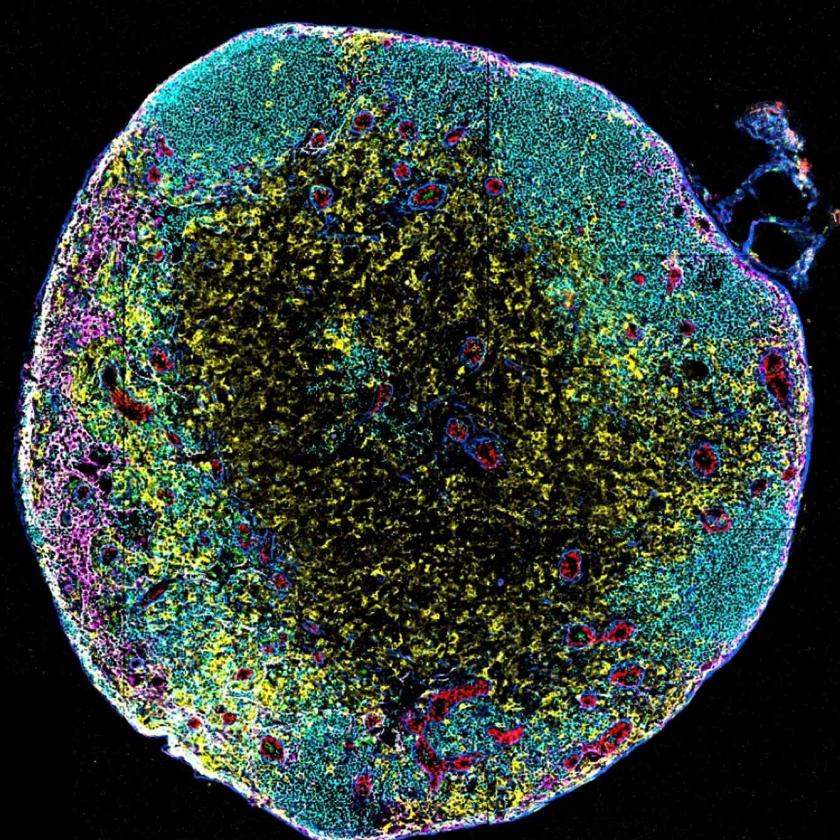
Novel Tools to Track and Manipulate Immune Cells in Autoimmunity Models
Principal Investigator: Susan R. Schwab, PhD
Autoimmune diseases result from a cascade of aberrant cell-cell interactions that ultimately cause tissue damage, but it has been difficult to determine which interactions are important within complex tissue environments. This project seeks to build a tool that will enable cells to effectively label their neighbors—which will be invaluable to our understanding of pre-clinical models and targets of autoimmune disease.
Early Detection and Diagnosis of Autoimmune Diseases Using Foundation AI Models
Principal Investigators: Aristotelis Tsirigos, PhD; Morgan Grams, MD, PhD; and Eric K. Oermann, MD
This project focuses on improving early detection and diagnosis of autoimmune diseases by applying self-supervised AI techniques to multi-modal electronic health record data. By integrating patient history, lab results, and imaging, we aim to develop a foundation AI model capable of identifying disease subgroups and recommending early diagnostic tests and treatments, ultimately enhancing precision medicine for autoimmune diseases. This mechanism is part of the first cross-center Colton Consortium collaboration in AI with Tel Aviv University and the University of Pennsylvania investigators.
Past Grant Awards
In recent years, the Judith and Stewart Colton Center for Autoimmunity has been supporting autoimmunity research at NYU Langone through multiple projects focused on some of the most relevant challenges in the field.
2023 Grant Awards

2022 Grant Awards

2021 Grant Awards
2020 Grant Awards

2019 Grant Awards

2018 Grant Awards