Department of Psychiatry Research
Donald C. Goff, MD
Marvin Stern Professor and Vice Chair for Research
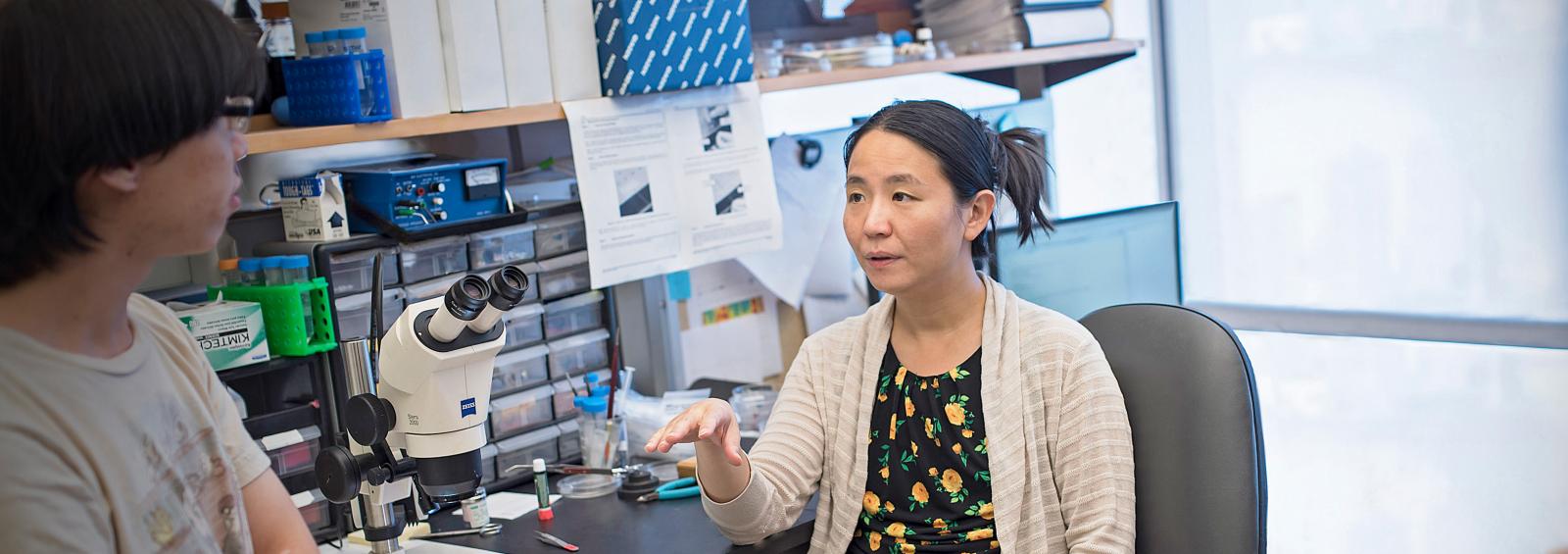
The Department of Psychiatry at NYU Langone is a world leader in research, with a long-standing mission of improving the mental health and wellbeing of adult patients experiencing a wide range of psychiatric illnesses. Our researchers are based at NYU Langone’s Tisch Hospital, NYC Health + Hospitals/Bellevue, the The Nathan S. Kline Institute for Psychiatric Research, the VA NY Harbor Healthcare System and the Manhattan Psychiatric Center. Our department fosters the career development of physician–scientists in addition to PhD researchers from many associated disciplines. Tanya C. Sippy, MD, PhD, director of research track for the psychiatry residency training program, and Naomi M. Simon, MD, PhD, vice chair for faculty development and engagement, lead this effort.
NYU Grossman School of Medicine is No. 6 in the country in National Institutes of Health psychiatry research funding, according to the Blue Ridge Institute for Medical Research.
Our department’s extensive research initiatives and resources reflect these rankings. Our scientific investigations encompass the following areas:
- adult attention deficit hyperactivity disorder
- anxiety, stress, and prolonged grief
- alcohol use disorder and traumatic stress
- brain aging and sleep
- computational research
- decision-making and reward
- dementia and neurodegenerative disease
- epidemiology
- mood disorders and cognition
- neuroscience
- obsessive–compulsive disorder
- post-traumatic stress disorder
- psychedelic medicine
- schizophrenia
- substance use disorder
Among our many research resources is a departmental biostatistics team dedicated to improving the way in which clinical trials can inform precision medicine. Through novel statistical analysis of biomarkers and other patient data, our research faculty aim to optimize personalized psychiatric care by pinpointing which individuals respond to specific treatments. Our investigators also have access to NYU Langone’s scientific cores and shared resources, the Clinical and Translational Science Institute, and other facilities.
Our broad research expertise leads to publication in a wide array of prestigious peer-reviewed journals. Our faculty have also contributed to textbooks in the field, such as Post-Traumatic Stress Disorder co-authored by department chair Charles R. Marmar, MD, and the chapter “Sensory Processing and Intolerance in OCD,” co-authored by associate professor Emily R. Stern, PhD, in Obsessive-compulsive Disorder: Phenomenology, Pathophysiology, and Treatment.
All of these efforts inform and advance patient care and make our department an excellent place for medical students, residents, fellows, doctoral students, and postgraduates to receive research training in psychiatry.
Publications

Research Faculty
