Annual Medical Education Innovations & Scholarship Conference Past Highlights
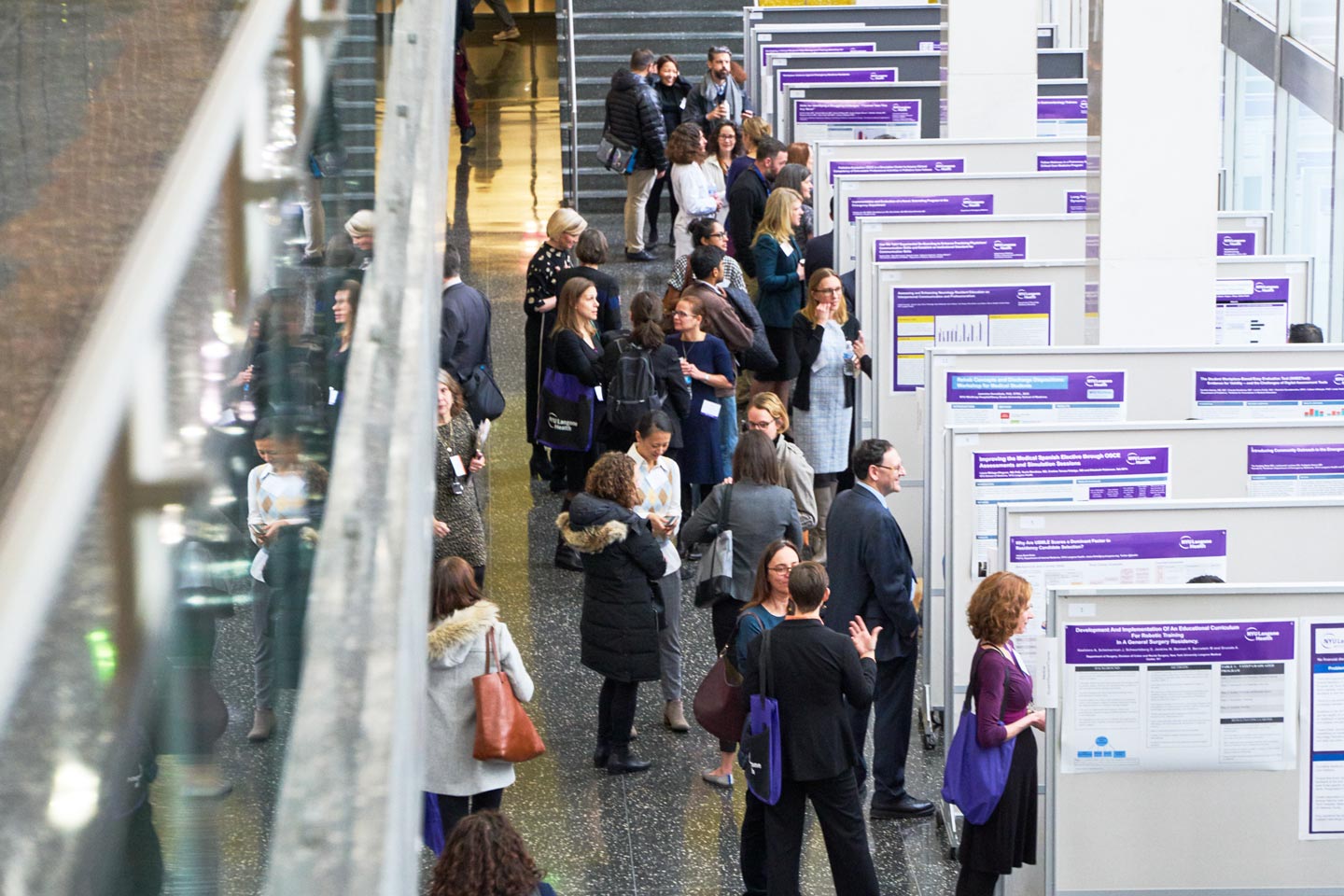
The Educator Community’s Annual Medical Education Innovations and Scholarship Conference recognizes the innovations occurring across NYU Grossman School of Medicine in undergraduate, graduate, and continuing medical education. The full-day program typically includes a poster session and workshops, and celebrates our faculty educators for their leadership and contributions to medical education. Attendees include faculty, students, residents, and staff from throughout our institution.
Here are highlights from past events.
2023 Annual Medical Education Innovations & Scholarship Conference Highlights
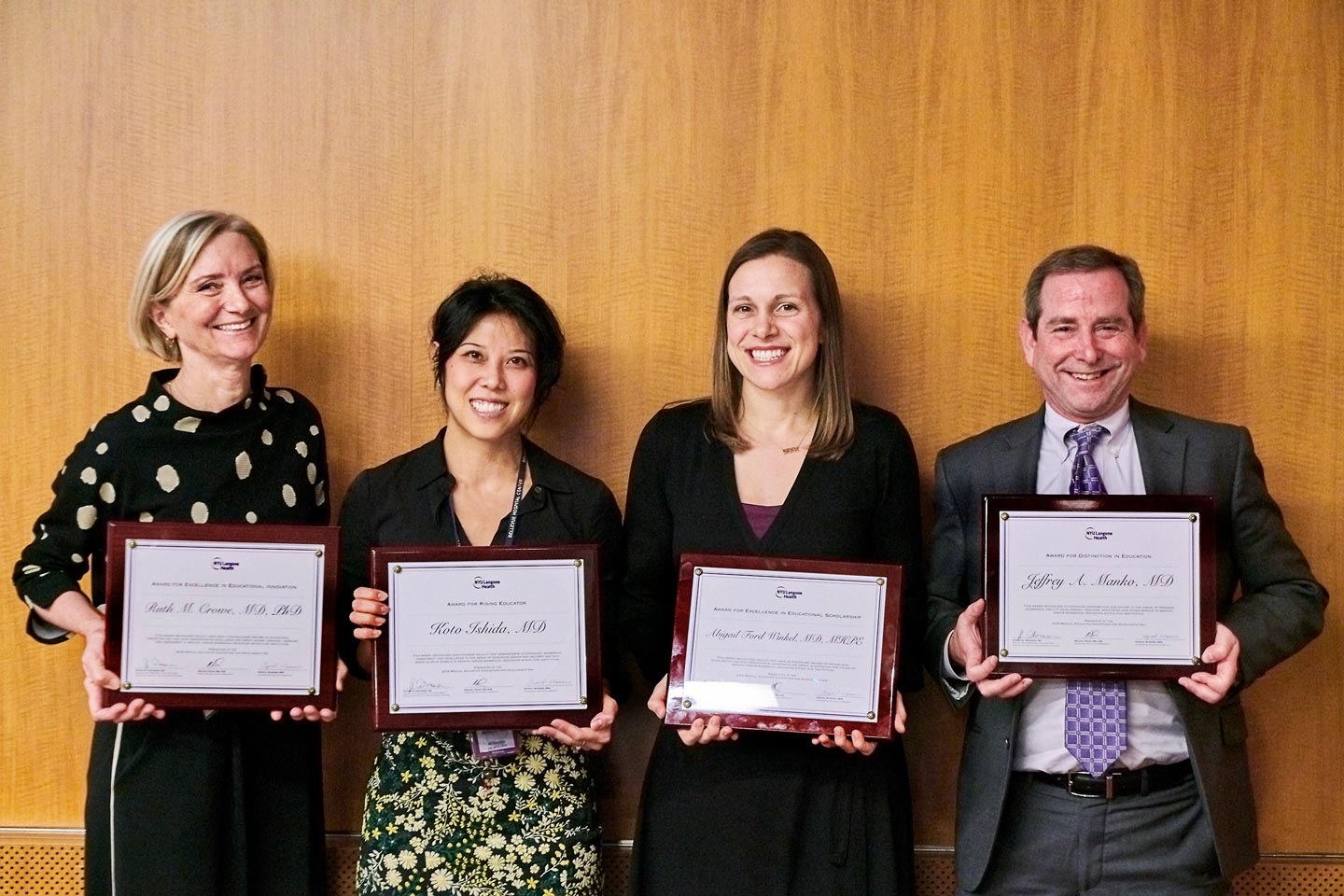
Our Eighth Annual Medical Education Innovations and Scholarship Conference featured more than 55 presentations and workshops, and an informative session with keynote speaker Adam Rodman, MD, MPH, instructor in medicine at the Beth Israel Deaconess Medical. Awards were also presented to recognize faculty at NYU Grossman School of Medicine for their outstanding contributions to medical education.
Crystal Mainiero, MPA, Steven Abramson, MD, and Michael Poles, MD, PhD, kicked off the event with a welcome address followed by a series of sessions that showcased the incredible work being conducted at NYU Grossman School of Medicine.
2022 Annual Medical Education Innovations and Scholarship Conference
Our Seventh Annual Medical Education Innovations and Scholarship Conference featured more than 60 presentations and workshops, a panel on “Harnessing Data and Analytics for Precision Medical Education,” and an informative session with keynote speaker Bill Cutrer, MD, MEd, associate dean for undergraduate medical education at Vanderbilt University School of Medicine.
Crystal Mainiero, MPA, and Michael Poles, MD, PhD, kicked off the event with a welcome address followed by a series of sessions that showcased the incredible work being conducted at NYU Grossman School of Medicine.
2021 Annual Medical Education Innovations and Scholarship Conference
Our Sixth Annual Medical Education Innovations and Scholarship Conference was virtual and featured 50 presentations and workshops; an informative Q & A session with guest speaker, Rochelle Walensky, MD, MPH, director of the Centers for Disease Control and Prevention (CDC); and a panel of experts on “Lessons Learned in Education During the Time of COVID.” Crystal Mainiero, MPA; Michael Poles, MD, PhD; and Steven Abramson, MD, kicked off the event with a welcome address followed by a series of sessions that showcased the extraordinary work being conducted at NYU Grossman School of Medicine.
We were honored to have Dr. Walensky, the 19th director of the CDC, as our special guest. The Q & A session was moderated by Jonathan LaPook, MD, the Mebane Professor of Gastroenterology and founder of The Empathy Project
A panel covering an array of important topics on “Lessons Learned in Education During the Time of COVID” was moderated by Joan F. Cangiarella, MD, former senior associate dean for education, faculty, and academic affairs.
2020 Annual Medical Education Innovations and Scholarship Conference
More than 3,000 attendees joined us virtually for our 2020 event, which focused on lesson learned from virtual teaching. The event, which began with a recap of the year from Ms. Crystal Mainiero, MPA; Michael Poles, MD, PhD; and Marc M. Triola, MD, also featured an interview with Dr. Anthony S. Facui and other highlights.
While the pandemic has presented challenges to educating our medical students, our accomplishments included innovations such as tele-simulation and moving the clinical curriculum to a virtual format.
2019 Annual Medical Education Innovations and Scholarship Conference
Our 2019 event, which attracted more than 300 attendees, featured an interview with Daniel Kahneman, PhD, recipient of the 2002 Nobel Memorial Prize in Economic Sciences, and David M. Oshinsky, PhD, the 2006 winner of the Pulitzer Prize in History for Polio: An American Story. The full-day program also included a poster session with 68 posters, 5 concurrent workshops, and awards that honor our faculty educators for their leadership and accomplishments.

Highlights from the event, which kicked off with welcome remarks from Steven Abramson, MD, and Ms. Crystal Mainiero, included the following presentations.
2018 Annual Medical Education Innovations and Scholarship Conference
The 2018 Annual Medical Education Innovations and Scholarship Conference featured a keynote address from George E. Thibault, MD, the former president of the Josiah Macy Jr. Foundation. “Reflections of a Foundation President: A Decade of Promoting Change in Health Professions Education,” gave insight into lessons learned, future levers for change, and strategic directions in health professions education. More than 150 attendees turned out for the day.